Every year, billions of doses of flu vaccine are administered to people around the world. But by the following year, the virus has mutated, and we need to create another vaccine to deal with the new strain.
New research by Tijana Ivanovic, assistant professor of biochemistry at Brandeis University, and several colleagues suggests the flu virus may owe its persistence at least in part to string-shaped structures called filamentous particles.
Ivanovic believes that developing an antiviral treatment to target these particles could help rid the world of flu for good.
The research appears in Nature Microbiology. The findings also apply to emerging viruses, such as avian flu and Ebola, but not to COVID-19, which has a different structure.
Researchers first discovered filamentous virus particles in 1946. They were shown to exist side-by-side with another type of viral particle that was sphere-shaped.
But when scientists cultured the flu virus in their labs, observing it undergo several replication cycles, the filamentous particles disappeared from view.
“This is what made it so difficult to dissect their function,” Ivanovic says. “They were elusive, so impossible to study.”
The researchers used a unique method to study the flu virus. It involves producing virus particles in the lab, observing them using a technique called total internal reflection fluorescence microscopy (TIRFM), and conducting computer simulations.
Ivanovic says her approach results in a more accurate and detailed account of the flu virus’s behavior than the methods used by scientists in the past.
Her method led to the following picture of spherical and filamentous particles:
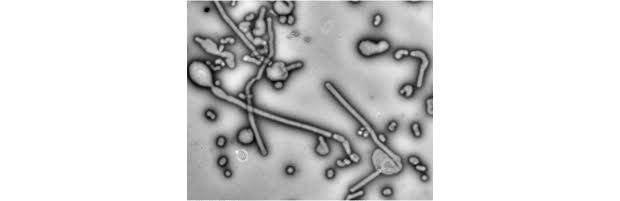
The flu virus relies on spherical particles to initially infect our cells. But then the immune system kicks in or we receive a vaccine, and that largely deactivates the spherical particles.
At this point, you return to full health and are considered cured of the virus. But the filamentous particles could still continue to infect your cells, having evaded the body’s defense system.
They can do this for a straightforward reason: they are a hundred to a thousand times bigger than the spherical ones. It’s a lot harder for the immune system’s antibodies to fight them.
Both spherical and filamentous particles have glycoproteins on their surface, critical in enabling the virus to enter cells. Ivanovic and her team found that 95% of the glycoproteins in filamentous particles can be deactivated, yet the particles will still function. Spherical particles don’t have that kind of staying power.
The persistence of the filamentous particles allows them to replicate and mutate. This doesn’t mean you’ll get sick again. The chances are overwhelming that the virus inside you won’t evolve enough to become harmful. It may mutate, but the immune system will still be able to fight it.
But since influenza infects tens of millions of people worldwide every year, the odds are good enough for the virus to mutate into a new strain in enough people to once again emerge as a global health threat.
Ivanovic says her research shows the need to develop a treatment that can target filamentous particles.
“We have to figure out a way to target the virus as a whole,” she says, “spherical and filamentous particles included.”
Additional coauthors are from Brandeis and the Albert Einstein College of Medicine in New York.
Source: Brandeis University
Original Study DOI: 10.1038/s41564-021-00903-1
Republished from Futurity